Home Tags Posts tagged with "brain cells"
brain cells
According to a report in the journal Stem Cell Research and Therapy, a spice commonly found in curries may boost the brain’s ability to heal itself.
The German study suggests a compound found in turmeric could encourage the growth of nerve cells thought to be part of the brain’s repair kit.
Scientists say this work, based in rats, may pave the way for future drugs for strokes and Alzheimer’s disease.
However, researchers say more trials are needed to see whether this applies to humans.
Researchers from the Institute of Neuroscience and Medicine in Julich, Germany, studied the effects of aromatic-turmerone – a compound found naturally in turmeric.
Rats were injected with the compound and their brains were then scanned.
Particular parts of the brain, known to be involved in nerve cell growth, were seen to be more active after the aromatic-turmerone infusion.
Scientists say the compound may encourage a proliferation of brain cells.

Turmerone, a spice commonly found in curries, may boost the brain’s ability to heal itself
In a separate part of the trial, researchers bathed rodent neural stem cells (NSCs) in different concentrations of aromatic-tumerone extract.
NSCs have the ability to transform into any type of brain cell and scientists suggest they could have a role in repair after damage or disease.
Dr. Maria Adele Rueger, who was part of the research team, said: “In humans and higher developed animals their abilities do not seem to be sufficient to repair the brain but in fish and smaller animals they seem to work well.”
The research found the higher the concentration of aromatic-turmerone, the greater the growth of the NSCs.
And the cells bathed in the turmeric compound seemed to specialize into certain types of brain cells more rapidly too.
Dr. Maria Adele Rueger added: “It is interesting that it might be possible to boost the effectiveness of the stem cells with aromatic-turmerone.
“And it is possible this in turn can help boost repair in the brain.”
She is now considering whether human trials may be feasible.
Aromatic-turmerone is the lesser-studied of two major compounds in turmeric that may have an effect on the human body.
Previous studies suggest the other compound, curcumin, could reduce inflammation in the body and have anti-cancer benefits.
A new research suggests that sleep loss may be more serious than previously thought, causing a permanent loss of brain cells.
In mice, prolonged lack of sleep led to 25% of certain brain cells dying, according to a study in The Journal of Neuroscience.
If the same is true in humans, it may be futile to try to catch up on missed sleep, say scientists at the University of Pennsylvania School of Medicine.
They think it may one day be possible to develop a drug to protect the brain from the side-effects of lost sleep.

Sleep loss may be more serious than previously thought, causing a permanent loss of brain cells
The study looked at lab mice that were kept awake to replicate the kind of sleep loss common in modern life, through night shifts or long hours in the office.
The research team studied certain brain cells which are involved in keeping the brain alert.
After several days of sleep patterns similar to those followed by night workers – three days of night shifts with only four to five hours sleep in 24 hours – the mice lost 25% of the brain cells, in part of the brain stem.
The researchers say this is the first evidence that sleep loss can lead to a loss of brain cells.
But they add that more work needs to be done to find out if people who miss out on sleep might also be at risk of permanent damage.
In the long-term, they think it might be possible to develop a medicine that protects brain cells, by boosting a natural chemical involved in sleep recovery.
A group of brain cells called tanycytes, which were identified as having the power to control appetite, could be the major cause of eating disorders such as obesity, a new research suggests.
In experiments in rodents, tanycytes were found to produce neurons which specifically regulate appetite.
The University of East Anglia (UEA) researchers say their find means appetite is not fixed at birth.
The new study is published in the Journal of Neuroscience.

A group of brain cells called tanycytes, which were identified as having the power to control appetite, could be the major cause of eating disorders such as obesity
It was previously thought that nerve cells in the brain associated with appetite regulation were generated entirely during an embryo’s development in the womb and could not be altered.
However, the UEA study’s discovery of these tanycytes, which act like stem cells, in the brains of young and adult rodents shows that appetite can be modified.
Researchers looked in detail at the hypothalamus section of the brain, which is known to regulate sleep, energy expenditure, appetite, thirst and many other critical biological functions.
They studied the nerve cells that regulate appetite using a “genetic fate mapping” technique and found that some cells added neurons to the appetite-regulating circuitry of the mouse brain after birth and into adulthood.
Dr. Mohammad Hajihosseini, from the university’s school of biological sciences, who led the research, said the discovery could eventually offer a permanent solution for tackling obesity – but it would take up to five or 10 years to translate the findings into humans.
“This study has shown that the neural circuitry that controls appetite is not fixed in number and could possibly be manipulated numerically to tackle eating disorders.
“The next step is to define the group of genes and cellular processes that regulate the behaviour and activity of tanycytes.
“This information will further our understanding of brain stem cells and could be exploited to develop drugs that can modulate the number or functioning of appetite-regulating neurons.”
Although there isn’t one single solution to controlling appetite, Dr. Mohammad Hajihosseini says any sustained solution to obesity must focus on the part of the brain that makes decisions on appetite.
“This is adding another piece to the jigsaw.”
The research was funded by the Wellcome Trust.
According to new studies, a daily multivitamin tablet may boost the memory and slow mental decline.
Taking supplements has a beneficial effect on memory and may work by increasing efficiency of brain cells.
One study showed that after just four weeks there were measurable changes in electrical activity in the brain when carrying out memory tests, not seen in a comparison group taking a placebo pill.
The body needs 13 vitamins to function properly and maintain health.
Vitamins A, C, D, E and K and the eight B vitamins each have specific job in the body.
Vitamin C keeps cells healthy, D regulates calcium and E maintains cell structure, while the B vitamins, including folic acid, have a wide range of functions.
One study at Monash University in Australia looked at whether multivitamins can improve cognitive abilities, and involved 3,200 men and women.
The results showed that those who used a multivitamin had improved ability to recall events or information.
The second study at Australia’s Swinburne University looked at women aged over 64 who had complained about poor memory.
Results showed that those taking a multivitamin supplement had improved rates of electrical activity in the brain while carrying out a memory test.
Researchers say it may work by increasing nerve cells’ efficiency and improving memory.
Professor David Kennedy, of the Brain, Performance and Nutrition Research Centre at Northumbria University, said: “The evidence is still limited but the studies hint at some possible beneficial effects.
“Optimal brain function depends on an adequate level of all of the vitamins. Multivitamins are likely to be more effective because people have different deficiencies.”
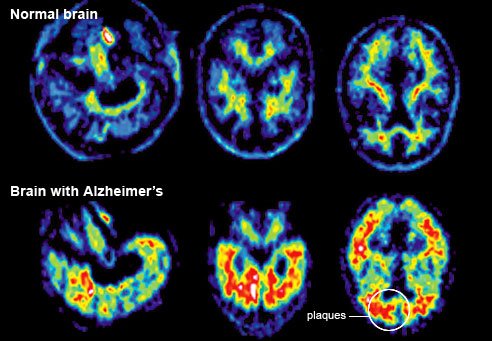
A team at Washington University School of Medicine has assembled a “timeline” of the unseen progress of Alzheimer’s before symptoms appear.
Scientists looked at families with a genetic risk of the disease.
Writing in the New England Journal of Medicine, they say signs appeared up to 25 years before the expected onset of the disease.
The 128 people in the study, from the UK, US and Australia, had a 50% chance of inheriting one of three mutations that are certain to cause early Alzheimer’s, which often develops in people’s 30s and 40s – much earlier than the more common form of Alzheimer’s which generally affects people in their 60s.
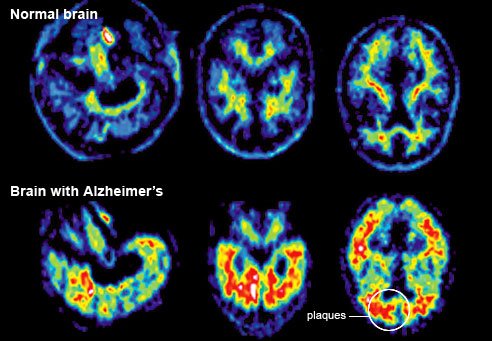
A team at Washington University School of Medicine has assembled a "timeline" of the unseen progress of Alzheimer's before symptoms appear
Those who carry the mutations will go on to develop the disease.
The researchers looked at the age the participants’ parents were when they developed the disease – and therefore how many years it was likely to be before they too showed symptoms.
They underwent blood and spinal fluid tests as well as brain scans and mental ability assessments.
The earliest change – a drop in spinal fluid levels of the key ingredient of Alzheimer’s brain plaques – can be detected 25 years before the anticipated age of disease onset, they suggest.
At 15 years, raised levels of tau, a structural protein in brain cells can be seen in spinal fluid – and shrinkage can also be detected within parts of the brain.
Changes in the brain’s use of the sugar glucose and slight memory problems become apparent 10 years before symptoms would appear, they suggest.
Researchers also tested other members of the families without the inherited mutations – and found no changes in the markers they tested for.
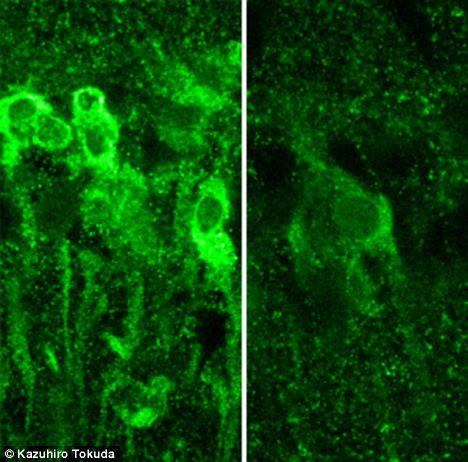
It was often said that alcohol killing off brain cells is behind the blackouts, but according to a new study what’s actually happening is that booze is preventing new memories being recorded in the first place.
Yukitoshi Izumi, research professor of psychiatry at Washington University School of Medicine in St. Louis, said: “We’ve found that exposure to alcohol inhibits some receptors and later activates others, causing neurons to manufacture steroids that inhibit memory formation.”
The brain cells affected by alcohol are found in the hippocampus and other brain structures involved in advanced cognitive functions.
Yukitoshi Izumi studied slices of the hippocampus from the rat brain.
When he treated hippocampal cells with moderate amounts of alcohol, the key areas for memory formation were unaffected, but exposing the cells to large amounts of alcohol inhibited the memory formation mechanism.
“It takes a lot of alcohol to block memory,” said senior investigator Charles F. Zorumski.
“But the mechanism isn’t straightforward. The alcohol triggers receptors to behave in seemingly contradictory ways, and that’s what actually blocks the neural signals that create memories. It also may explain why individuals who get highly intoxicated don’t remember what they did the night before.”
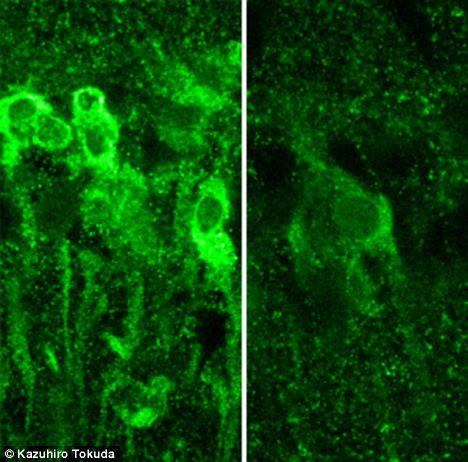
Neurons in the hippocampus exposed to large amounts of alcohol produce steroids, which inhibit the formation of memory (left), vs. normal neurons (right)
The study is echoed by the work of researchers at the University of California, San Diego, who found that some people are actually more prone to blackouts than others.
“Our study’s findings suggest that some people are more likely to experience alcohol-induced blackouts than others due to the way alcohol affects brain activity in areas involved in self-monitoring, attention, and working memory,” said lead author Reagan R. Wetherill.
“Some people may be more vulnerable to alcohol’s effects than others. In other words, just because your friend may be able to drink a certain number of drinks and appear to be functioning fine, it does not mean that you or everyone else can.”
“Blackouts”, where very heavy drinkers wake up and are unable to remember anything that happened, are quite rare, says Reagan R. Weatherill – but their cousin, the “brown out”, where details vanish, is much more common.
The study – using 24 students, 12 of whom suffered “brown outs” while drinking, and 12 who did not, challenged the students to complete memory exercises both while drunk and while sober.
The study found that the students had similar abilities to remember and to multi-task while sober – but alcohol acted as a “magic switch” for some which stopped them remembering.
It suggests there is a biochemical trigger for some people to forget what happens while drinking.
“Through use of imaging technology, this study has made the really intriguing finding that the unique patterns of blood flow and neural activity seen in persons prone to experience those amnestic phenomena emerged only after they became intoxicated,” she said.
“That finding, taken together with results from prior research on fragmentary blackouts, suggests there are individual differences in how alcohol impacts memory.”
“Alcohol intoxication reduced activity in a brain region involved in <<multitasking>>,” said Reagan R. Wetherill.
“Thus, alcohol appears to affect a person’s ability to multitask, and also affects some people’s ability to engage brain areas required for encoding and remembering previous experiences.”
“Irrespective of the specific type of alcohol-related memory loss involved, if one is experiencing blackouts it is an important signal that negative personal and health consequences are more likely to occur.
“Not fully recalling one’s life experiences, particularly those that occur while one is intoxicated, creates a state of vulnerability where the chances increase for the individual to incur all kinds of problems.”
Researchers studying mice at the Stanford University School of Medicine in California have converted skin cells directly into cells which develop into the main components of the brain.
The experiment, which was reported in Proceedings of the National Academy of Sciences, skipped the middle “stem cell” stage in the process.
The researchers said they were “thrilled” at the potential medical uses.
Far more tests are needed before the technique could be used on human skin.
Stem cells, which can become any other specialist type of cell from brain to bone, are thought to have huge promise in a range of treatments. Many trials are taking place, such as in stroke patients or specific forms of blindness.
One of the big questions for the field is where to get the cells from. There are ethical concerns around embryonic stem cells and patients would need to take immunosuppressant drugs as any stem cell tissue would not match their own.
An alternative method has been to take skin cells and reprogram them into “induced” stem cells. These could be made from a patient’s own cells and then turned into the cell type required, however, the process results in cancer-causing genes being activated.
The research group is looking at another option – converting a person’s own skin cells into specialist cells, without creating “induced” stem cells. It has already transformed skin cells directly into neurons.
This study created “neural precursor” cells, which can develop into three types of brain cell: neurons, astrocytes and oligodendrocytes.
These precursor cells have the advantage that, once created, they can be grown in a laboratory into very large numbers. This could be critical if the cells were to be used in any therapy.
Brain cells and skin cells contain the same genetic information, however, the genetic code is interpreted differently in each. This is controlled by “transcription factors”.
The researchers used a virus to infect skin cells with three transcription factors known to be at high levels in neural precursor cells.
After three weeks about one in 10 of the cells became neural precursor cells.
Lead researcher Prof. Marius Wernig said: “We are thrilled about the prospects for potential medical use of these cells.
“We’ve shown the cells can integrate into a mouse brain and produce a missing protein important for the conduction of electrical signal by the neurons.
“More work needs to be done to generate similar cells from human skin cells and assess their safety and efficacy.”
Dr. Deepak Srivastava, who has researched converting cells into heart muscle, said the study: “Opens the door to consider new ways to regenerate damaged neurons using cells surrounding the area of injury.”