Diabetes may begin in the bowel, new study suggests
A new study, published this week in the journal Cell Host & Microbe, indicates that bowel may play an important role in the development of diabetes.
This is a new and somehow surprising approach to diabetes, since until now most of the studies have focused on pancreas and liver. Pancreas produces insulin, the hormone that regulates sugar (glucose) blood levels and liver is the main organ where the sugar is stored.
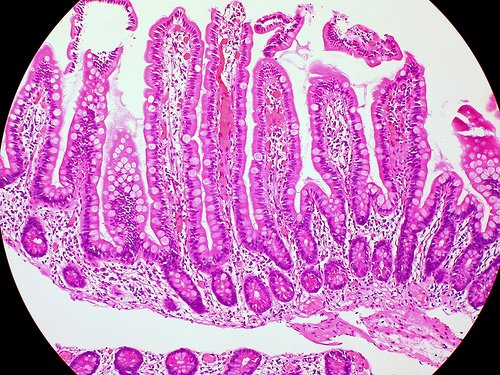
Normally, a mucus layer lines inside the intestines (small intestine and colon) to protect the organism from infection (with bacteria, viruses, fungi, parasites) and to keep the balance, or homeostasis of the host-microbiota (good bacteria). The bacteria that naturally live in the colon (host-microbiota, or gut flora) help digest food and synthesize vitamins.
On the other hand, bacteria from intestines can produce toxins and carcinogens, and cause multisystem organ failure, sepsis, colon cancer, and inflammatory bowel disease (IBD).
Intestinal bacteria also influence the BMI (body mass index). Obese persons have especially bacteria called Firmicutes in their bowel, while lean people have Bacteroidetes. These bacteria are involved in the digestion of fatty acids and polysaccharides. In other study obese mice were transplanted into germ-free recipient, and as a result they gain weight despite a decrease in food consumption.
An important factor in health is the balance of bacterial numbers.
If the normal intestinal mucus barrier is altered, this may lead to inflammation and diabetes.
The integrity of the intestinal mucus barrier, made of lipids, proteins and glycoproteins, may play a role in developing insulin resistance and in diabetes.
The researchers of Washington University School of Medicine in St. Louis, including specialists in gastroenterology and genome sciences, have tried to determine what happens in mice that were unable to produce fatty acid synthase (FAS) in their intestines.
The enzyme FAS is essential for lipids production, therefore essential for mucus secretion, it regulates the production of a mucus component Mucin 2.
FAS secretion is regulated by insulin, and as a consequence people with diabetes have faulty FAS.
“Diabetes may indeed start in your gut. When people become resistant to insulin, as happens when they gain weight, FAS doesn’t work properly, which causes inflammation that, in turn, can lead to diabetes,” said Dr. Clay F. Semenkovich, study author.
Mice became sick, they had diarrhea and other symptoms. The changes in their gut flora made the mice sick, thought the scientists at the beginning, but after a detailed analysis those changes did not prove to be the cause.
Mice have developed chronic inflammation in their guts. Intestinal inflammation is a powerful predictor of diabetes.
“The first striking thing we saw was that the mice began losing weight. They had diarrhea and other gastrointestinal symptoms, and when we looked closely at the tissue in the gut, we found a lot of inflammation,” said Dr. Xiaochao Wei, study author.
“The mice had substantial changes in their gut microbiome. But it wasn’t the composition of microbes in the gut that caused the problems,” said Dr. Clay F. Semenkovich.
The mice were sick because of a defect in fatty acid synthase. They had lost the protective lining of mucus in the intestines and bacteria could invade intestinal cells.
Those gastrointestinal effects were similar to inflammatory bowel disease. Helpful bacteria can be very harmful to the organism if they get outside of the digestive tract (when the intestine is perforated, or becomes permeable, in disease like cirrhosis).
Prior to this observation, other reports have shown that colon biopsies from patients with ulcerative colitis had low amounts of fatty acid synthase.
“Fatty acid synthase is required to keep that mucosal layer intact. Without it, bad bacteria invade cells in the colon and the small intestine, creating inflammation, and that, in turn, contributes to insulin resistance and diabetes, ” said Dr. Xiaochao Wei.
Inflammatory substances can cause insulin resistance and inhibit the secretion of insulin, and may lead to diabetes. On the other hand, insulin resistance promote inflammation.
Lots of people with diabetes not only have inadequate FAS, but they also have gastrointestinal disorders, said Dr. Clay F. Semenkovich.
“Abdominal pain and diarrhea are some of the most common problems we see in people with diabetes. We could only connect these ‘dots’ because other experts at the university could help us link what we observed in these mice to what occurs in patients with diabetes and inflammatory bowel disease,” he said.
FAS and Mucin 2 may be potential targets for diabetes therapy. However, further studies are needed, and the scientists plan to study how the secretion of FAS is affected in people with diabetes.
