Home Tags Posts tagged with "Lancet Oncology"
Lancet Oncology
A new research has found that a healthy lifestyle may do more than simply slow the ageing process – it could actually reverse it.
Keeping physically fit, having a plant-based diet and practicing stress-reduction techniques such as yoga could extend the lifespan of cells, researchers say.
They studied the effect of healthy living on lengths of DNA called telomeres – tiny “caps” on the ends of chromosomes that protect against the ageing process.
Just as the tips of shoelaces prevent fraying, telomeres keep chromosomes stable and prevent deterioration when the cells containing them divide.
Dubbed the “chromosomal clock”, they shorten as we age. This process is associated with a greater risk of early death and of conditions such as heart disease, dementia, diabetes and cancers, as well as with increased vulnerability to infection.
Scientists believe the shortening process may even place an unextendable limit on the human lifespan.

Healthy lifestyle may do more than simply slow the ageing process
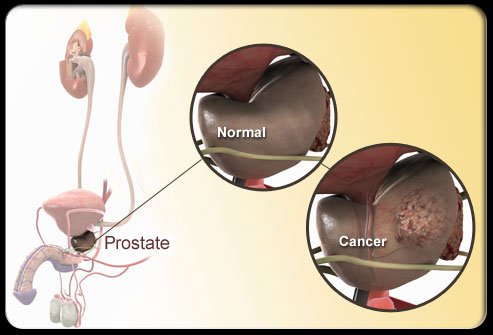
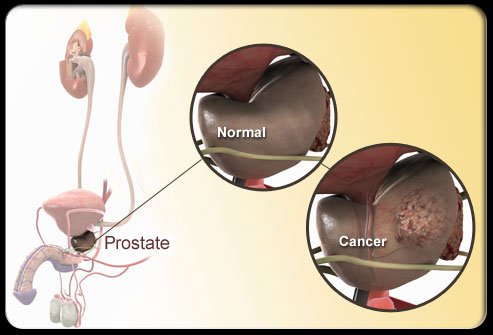
The pilot study, published in The Lancet Oncology, compared two groups of men with early non-aggressive prostate cancer who had not undergone surgery or radiotherapy but were having regular checks.
One group of 25 men continued without making any changes. Ten others underwent a radical lifestyle transformation supervised by doctors, nutritionists and psychologists.
Their diet was switched to one high in plant proteins, fruits, vegetables and unrefined grains while low in fat and processed carbohydrates. They were taught stress reduction techniques such as yoga and meditation, and were given counseling. They also took moderate levels of exercise, such as walking for 30 minutes, six days a week.
After five years, blood tests showed that the telomeres of the healthy-lifestyle group had lengthened by an average of 10%, effectively reversing the natural ageing process. But the telomeres of the group who continued with their previous lifestyle shortened by an average of 3%.
The study found no significant difference between the groups in the progress of prostate cancer.
But the scientists believe that their findings carry an important health message with wider implications.
The team’s leader, Prof. Dean Ornish, from the Preventive Medicine Research Institute at the University of California in San Francisco, said: “The implications of this relatively small pilot study may go beyond men with prostate cancer.
“If validated by large-scale randomized controlled trials, these comprehensive lifestyle changes may significantly reduce the risk of a wide variety of diseases and premature mortality. Our genes, and our telomeres, are a predisposition, but they are not necessarily our fate.”
A new study has found that skin patches which deliver oestrogen into the blood may be a cheaper and safer treatment for prostate cancer than current therapies.
The main treatment is injections of a chemical to cut levels of testosterone – the driving force of many prostate cancers – but it causes side effects.
The Imperial College London study in the Lancet Oncology compared patches and injections in 254 patients.
It found patches were safe and should avoid menopause-like side effects.
Using oestrogen to treat prostate cancer is an old treatment.
Both oestrogen and testosterone are very similar chemically, so ramping up the levels of oestrogen in the body can reduce the amount of testosterone produced – and slow prostate cancer growth.

Skin patches which deliver oestrogen into the blood may be a cheaper and safer treatment for prostate cancer than current therapies
However, taking oral oestrogen pills caused significant health problems by overdosing the liver. The organ then produced chemicals which caused blood clots, heart attacks and strokes.
The preferred treatment is injections of a drug, LHRHa, which reduces the production of both oestrogen and testosterone. However, this has side effects similar to the menopause in women – resulting in poor bone health and diabetes.
Prof. Paul Abel, from Imperial College London, said: “We’re not claiming this is equivalent to current therapies yet, but it does look like we are getting castration levels of testosterone.”
However, the researchers need to follow patients for longer.
“The next step is to test if the oestrogen patches are as effective at stopping the growth of prostate cancer as the current hormone treatments, we’re now testing this in over 600 patients.”
Experts have found that a blood test that reads genetic results like a barcode can pick out the most aggressive prostate cancers.
The test, which looks at the signature pattern of genes switched on and off in blood cells triggered by the tumor, can sort the “tigers” from the “pussycats”.
London’s Institute of Cancer Research trialled the test in 94 patients.
The findings are published in the Lancet Oncology medical journal.
Prostate cancer is a very diverse disease – some people live with it for years without symptoms, but for others it can be aggressive and life-threatening.
Currently, doctors take a small sample of the tumor – a biopsy – to examine under a microscope to get a better idea of how dangerous
Experts hope that ultimately the barcode blood test could be used to make a more accurate estimation.
In the study, the scientists were able to split the patients into four groups based on the results of the barcode test. One of these groups fared far worse, surviving for significantly less time than the other patients.
The researchers then confirmed their findings in another 70 US patients with advanced cancer, which revealed that nine genes could accurately spot who had the least chance of survival.
Patients with this “bad” gene signature survived for an average of nine months compared with 21 months for those without it.
US researchers at the Dana-Faber Cancer Institute and the Memorial Sloan-Kettering Cancer Centre have also been testing a similar prostate cancer blood test.
Their six-gene test could split patients into high and low risk groups.
Prostate cancer is the most common male cancer in the UK, accounting for almost a quarter of male cancers.
Each year, nearly 35,000 men are diagnosed and more than 10,000 die from the disease.
British scientists have discovered that ultrasounds could treat early prostate cancer and may have far fewer side-effects than existing therapies.
A 41-patient study in the journal Lancet Oncology suggests targeted ultrasound treatment could reduce the risk of impotence and incontinence.
Researchers say it could transform future treatment if the findings are repeated in larger studies.
The Medical Research Council (MRC) in UK, which funded the study, welcomed the results, which it said were promising.
Each year 37,000 men in the UK are diagnosed with prostate cancer.
Many face a difficult dilemma: the disease kills about 10,000 men every year, but for some it may not get worse if left untreated.
Standard treatment with surgery or radiotherapy involves treating the whole prostate gland, and can harm surrounding tissue, with a serious risk of side-effects, including urinary incontinence and impotence.
British scientists have discovered that ultrasounds could treat early prostate cancer and may have far fewer side-effects than existing therapies
Doctors at University College Hospital in London have carried out the first trial using high-intensity focused ultrasound (HIFU) aimed at small patches of cancer cells on the prostate.
This was a “proof of concept” study involving 41 patients.
They used a probe, placed close to the prostate, which emits sound waves that heat the targeted cells to 80C, while causing minimal damage to surrounding nerves and muscles.
Hashim Ahmed, a urological surgeon at the trust who led the study, says the results, 12 months after treatment, are very encouraging.
“We’ve shown in this study that focal therapy – by targeting the individual areas of cancer – can avoid the collateral damage. We’ve shown that nine in 10 men had no impotence and none of the men in the study had incontinence of urine.”
Hashim Ahmed says the early evidence on cancer control is also very good. But he says this needs to be evaluated in much larger studies.
“This could offer a transformation of the way we treat prostate cancer. It could offer a cost-effective treatment for the NHS, and offer men with early prostate cancer an opportunity to treat their disease, but with very few side-effects.”
A patient on the trial, 72-year-old Robert Page, from Croydon, says his treatment, two years ago, was a great success.
“The outcome was very good,” he said.
“I was very pleased with the treatment and very happy with the lack of side-effects, particularly when I contrast that with what might have been the case if I’d had one of the other, alternative, treatments.”
The study was funded by the Medical Research Council, the Pelican Cancer Foundation and St Peter’s Trust.
Professor Gillies McKenna, director of the Gray Institute for Radiation Oncology and Biology, a joint collaboration between the MRC and Cancer Research UK, welcomed the findings.
“If these promising results can be confirmed in a randomized controlled trial, focal therapy could soon become a reasonable treatment choice for prostate cancer alongside other proven effective therapies.”
The chief executive of the Prostate Cancer Charity, Owen Sharp, also emphasized the importance of further research.
“We welcome the development of any prostate-cancer treatment which limits the possibility of damaging side-effects, such as incontinence and impotence. These early results certainly indicate that focal HIFU has the potential to achieve this in the future.
“However, we need to remember that this treatment was given to fewer than 50 men, without follow-up over a sustained period of time.
“We look forward to the results of further trials, which we hope will provide a clearer idea of whether this treatment can control cancer in the long term whilst ridding men of the fear that treating their cancer might mean losing their quality of life.”
A report on managing cancer costs, made by 37 cancer experts (economists, patient advocates and physicians) from developed countries (U.S., UK, Germany, Australia), was published in the Lancet Oncology on September 26 . The study highlights the need of a judicious medication for terminal cancer patient.
Professor Richard Sullivan, of the King’s Health Partners Integrated Cancer Centre, London, has presented the study at the European Multidisciplinary Cancer Congress in Stockholm.
Input from drug-makers, payers and educators will be key to future discussions, David Collingridge, the journal’s editor, said.
“With an aging global population and an endless conveyor belt of expensive new drugs and technologies and increasing financial pressures, the cost of cancer care in high-income countries is becoming unsustainable,” The Lancet Oncology said.
Developed countries have varying levels of GDP assigned to health, but the percent of cancer care cost is between four and seven in the majority of countries.
Around 12 million people worldwide are diagnosed with cancer annually, the costs of the new cases was at least $286 billion in 2009, according to the report. By 2030, about 22 million people will be diagnosed with the disease annually. More than half of the $286 billion in costs was related to treatment, while a quarter was linked to lost productivity.

"We over-diagnose, over-treat, and over-promise. This extends from use of complex technology, surgery, and drugs to events related to the acceptance of treatment side-effects." say experts, making a special reference to terminal cancer.
In UK around 310,000 people are diagnosed with cancer every year and by 2030 this is expected to have risen to 400,000. The National Health Service spends over £5billion annually on cancer treatments, up from £3billion in 2002.
“All health systems face budget limitations, while at the same time the cancer burden and expenditures are increasing steeply. Every cancer patient, now and in the future, must have fair access to quality cancer care and to innovation. This can only be safeguarded by transparent and evidence-based analysis and policy development,” said Professor Michael Baumann , president of the European cancer organization, ECCO.
The cancer experts have criticized a “culture of excess” that gives false hopes to patients with terminal cancer.
“In developed countries, cancer treatment is becoming a culture of excess. We over-diagnose, over-treat, and over-promise. This extends from use of complex technology, surgery, and drugs to events related to the acceptance of treatment side-effects.” the cancer experts said.
They emphasized the importance of choosing a right treatment strategy for terminal cancer patients. The life-extending medication should not be use as it shows no benefits for terminal cancer, and has dangerous side-effects.

The life-extending medication should not be use as it shows no benefits for terminal cancer, and has dangerous side-effects, said the cancer experts.
“Special consideration must be given to costs of cancer care at the end of life. Many forms of cancer are currently incurable and patients will eventually die from their disease.”
“In fact studies suggest that a substantial portion of the total cost of cancer care is for care delivered in the last weeks or days of life, and that much of this care is futile and potentially inconsistent with patients’ wishes.”
“If we could accurately predict when further disease-directed therapy would be futile, we clearly would want to spare the patient the toxicity and false hope associated with such treatment, as well as the expense.”
The scientists said a more rigorous evaluation of the relative benefits of surgery to treat cancer and of the less invasive robotic surgery had to be done.
Reducing the cost of cancer services or reducing the number of people using them, especially terminal cancer patients, are the two ways the authors proposed to solve the problem.
The best cancer treatments would be the preserve of the rich because they would be too expensive for the Health Service, warned last week Professor Karol Sikora, one of the 37 cancer experts.
Molecular bio-markers could be used to pre-screen patients for treatments and imaging methods should be used to select only those patients who could benefit from a treatment. Early-stage studies could also help to remove marginally effective or ineffective drugs faster, researchers said.
“We are at a crossroads for affordable cancer care, where our choices, or refusal to make choices, will affect the lives of millions of people. Making individual patients more sensitive to the costs of care is necessary for an informed public debate around this critical issue,” Professor Richard Sullivan said.

MRI performed prior to surgery predicts the follow-up treatment for advanced rectal cancer, recent study shows. Generally the doctors will not abandon drugs for terminal cancer patients, despite the costs.
Cancer diagnosis and treatment has became more complex, with imaging, surgery, radiation and drug therapy. Specialists need to come together and discuss with patients, insurers and industry players the best ways to lower costs without compromising care, they said.